Sexual activity is usually talked about in terms of pleasure, intimacy, and emotional connection. What’s discussed far less often is how it affects the urinary system — a quiet but essential part of the body that works closely alongside the reproductive organs. Understanding this connection can make a meaningful difference in long-term comfort, confidence, and overall wellbeing.
During sex, the body experiences increased blood flow, muscle movement, warmth, and moisture. These natural changes create ideal conditions for closeness and arousal, but they also allow bacteria to move more easily across nearby areas of skin. Microorganisms that are normally harmless can be transferred toward the urethra through friction and contact.
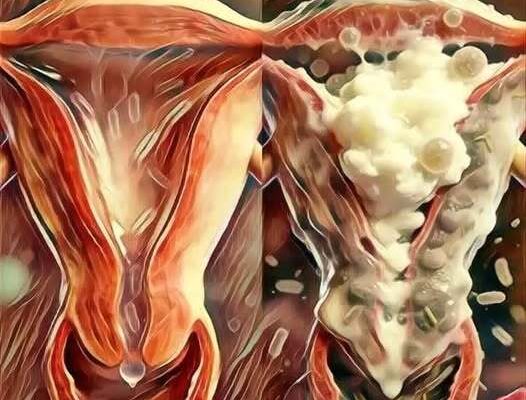
For women, this risk is higher because the urethra is short and located close to both the vaginal and anal openings. Even routine sexual activity can unintentionally introduce bacteria into the urinary tract. Men benefit from a longer urethra, which offers some protection, but they are not immune. Prolonged intercourse, dehydration, insufficient hygiene, or repeated encounters without recovery time can still allow bacteria to travel upward.
The urinary system is designed to filter waste, not fight frequent microbial exposure. While it has natural defenses, these can be overwhelmed when exposure is repeated or the body is already under stress. Recognizing this helps shift sexual health from a narrow focus on reproduction or infections to a more holistic understanding of how everyday intimacy affects the entire body.
Why Urination Matters More Than You Think
Once bacteria reach the urethra, the body relies heavily on urine flow to flush them out. Urinating helps dislodge microorganisms before they can attach to tissue or move into the bladder. When urination is delayed after sex, bacteria have time to settle, multiply, and form colonies — often without immediate symptoms.
This delayed response explains why many people struggle to identify the cause of urinary tract infections. Symptoms may appear hours or days later, leading people to blame stress, diet, or bad luck rather than subtle habits that accumulate over time. Dehydration concentrates urine, making it more irritating and less effective at cleansing. Ignoring the urge to urinate further increases risk.
Hormonal changes, fatigue, immune stress, and chronic conditions can also weaken the body’s defenses. Sexual activity itself isn’t harmful — but when combined with these factors, it can tip the balance toward infection. Understanding this removes fear and blame, replacing them with awareness and prevention.
Postcoital Cystitis: Common, Manageable, and Often Misunderstood
One of the most common urinary issues linked to sexual activity is postcoital cystitis — a bladder infection that develops after intercourse. It’s most often caused by E. coli, a bacterium that normally lives in the intestines but becomes problematic when it enters the urinary tract.
Symptoms may include burning during urination, frequent urges with little output, pelvic pressure, cloudy or strong-smelling urine, and sometimes fever or discomfort. Beyond physical pain, recurrent infections can take an emotional toll. Anxiety around intimacy may develop, and sex can become associated with discomfort rather than connection.
It’s important to emphasize that postcoital cystitis is common — especially among sexually active women — and it is not a sign of poor hygiene, carelessness, or personal failure. Understanding the biology behind it allows people to respond with practical solutions instead of shame or avoidance.
One Simple Habit That Makes a Big Difference
Urinating shortly after sex is one of the most effective and accessible ways to protect urinary health. This small action uses the body’s natural cleansing mechanism to flush out bacteria before they can cause problems.
Beyond infection prevention, postcoital urination helps reduce irritation, supports microbial balance, and relieves bladder pressure caused by increased blood flow and pelvic muscle engagement during sex. Unlike medications or supplements, this habit is free, noninvasive, and easy to incorporate into daily life.
Consistency is what makes it powerful. When practiced regularly, it significantly lowers infection risk for many people — proving that simple habits can have lasting benefits.
Supporting Urinary Health Through Everyday Choices
Urinary comfort isn’t shaped by one habit alone. Hydration plays a major role — drinking enough water dilutes urine, reduces irritation, and increases flushing frequency. Gentle cleansing of the genital area before and after sex can help, but harsh soaps, douching, or aggressive scrubbing should be avoided, as they disrupt natural protective barriers.
Breathable underwear allows moisture to evaporate, reducing bacterial growth. Avoiding long delays between bathroom visits prevents bacterial buildup. For those prone to recurrent issues, additional adjustments can help: using adequate lubrication to reduce friction, choosing positions that minimize urethral irritation, and maintaining mutual hygiene with partners.
These practices aren’t about limiting pleasure or creating anxiety around intimacy. They’re about working with the body — allowing it to recover, rebalance, and remain resilient over time.
A Healthier, More Informed Approach to Intimacy
Understanding how sexual activity influences urinary health encourages a more compassionate and realistic view of intimacy — one that values both emotional closeness and physical comfort. Sexual education often focuses on contraception and infections, while everyday physiological responses are overlooked.
Yet urinary discomfort can deeply affect confidence, mental health, and relationships. When people lack information, they may accept discomfort as inevitable or internalize it as personal failure. Knowledge changes that narrative.
With awareness and simple preventive habits, intimacy can remain a source of pleasure, trust, and connection — while also supporting long-term urinary and reproductive wellbeing. When care and understanding guide sexual health, the body is better equipped to stay balanced, comfortable, and strong.